Domestic and family violence has profound consequences on everyone involved—but children are among the most deeply and often invisibly affected. Though they may not always be the direct victims, simply witnessing violence, hearing shouting, or sensing fear can alter a child’s development and mental health in powerful ways. Children are not just bystanders in homes where domestic violence occurs; they are direct victims of a hostile environment.
This article explores how domestic violence impacts children across all areas of their lives: behavior, mental and physical health, learning, relationships, and long-term development. It also highlights the urgent need for trauma-informed care, supportive environments, and holistic interventions to break the cycle.
Understanding Exposure
Children are considered to be affected by domestic violence when they:
- Witness physical or emotional abuse of a parent or caregiver
- Hear arguments, threats, or violent acts
- See injuries or aftermaths of violent incidents
- Are used as tools of manipulation or emotionally coerced
- Experience direct abuse while living in a violent home
- Live in a state of chronic fear or hypervigilance
- Are exposed to controlling or intimidating behaviors
The Domestic Abuse Act 2021 in the UK, and similar reforms in Australia and elsewhere, now formally recognize children as victims in their own right—not merely witnesses—when domestic violence occurs at home.
Behavioral and Emotional Impacts

Children exposed to violence often display a wide range of behavioral and emotional symptoms, including:
- Aggression, hostility, and tantrums
- Withdrawal or running away
- Impulsive or risky behaviors
- Trouble regulating emotions
- Frequent mood swings or hyperactivity
Such behaviors are often misdiagnosed or misunderstood. Rather than labeling these children as “problematic,” it’s essential to recognize their behavior as trauma responses.
Emotional effects include:
- Fear, sadness, and anxiety
- Depression or suicidal thoughts
- Guilt or self-blame for the violence
- Emotional numbness or detachment
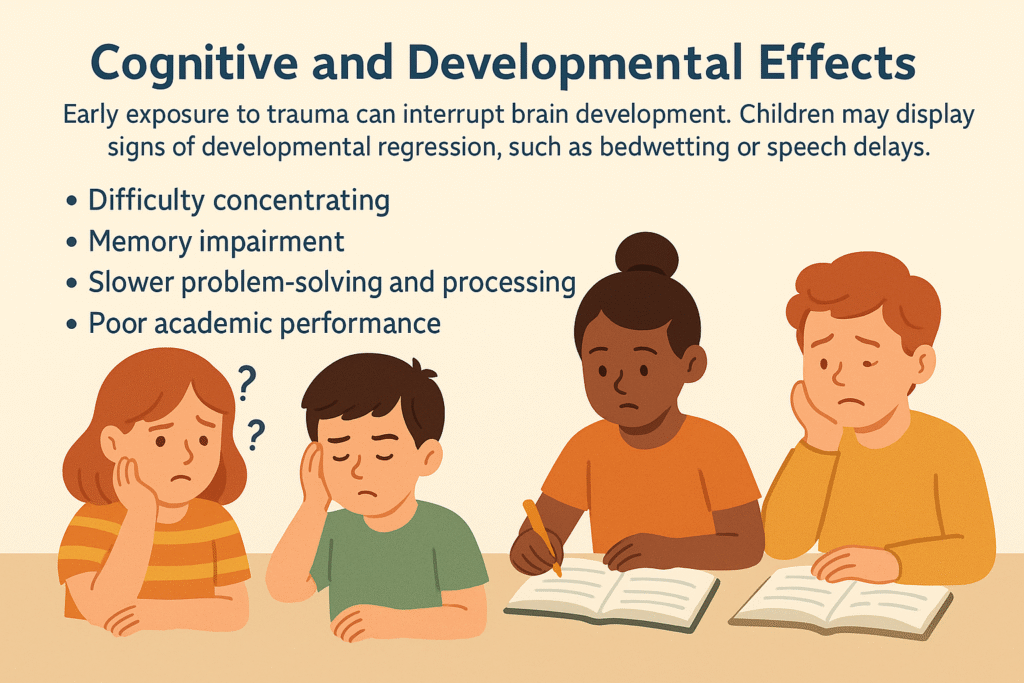
Cognitive and Developmental Effects
Early exposure to trauma can interrupt brain development. Children may display signs of developmental regression, such as bedwetting or speech delays.
Cognitive issues may include:
- Difficulty concentrating
- Memory impairment
- Slower problem-solving and processing
- Poor academic performance
Research from the Murdoch Children’s Research Institute found that children exposed to domestic violence are 2–3 times more likely to develop language delays, behavioral problems, and health issues by age ten.
Educational Challenges
Children living in violent homes often struggle in school due to the psychological toll of their home life:
- Poor concentration due to hypervigilance
- Chronic absenteeism
- Disruptive behavior in class
- Learning disabilities
- Reduced engagement or academic motivation
Teachers and school staff are often the first to notice these signs but may not connect them to domestic violence unless trained in trauma-informed care.
Social and Relational Difficulties
Children affected by domestic violence may struggle to build healthy relationships. They often:
- Display difficulty trusting others
- Push people away or become overly clingy
- Attach to unsafe peers or adults
- Imitate violent or controlling behavior in friendships or dating
These early relationship challenges can lead to lifelong social difficulties, including trouble with intimacy, boundaries, and emotional communication in adulthood.
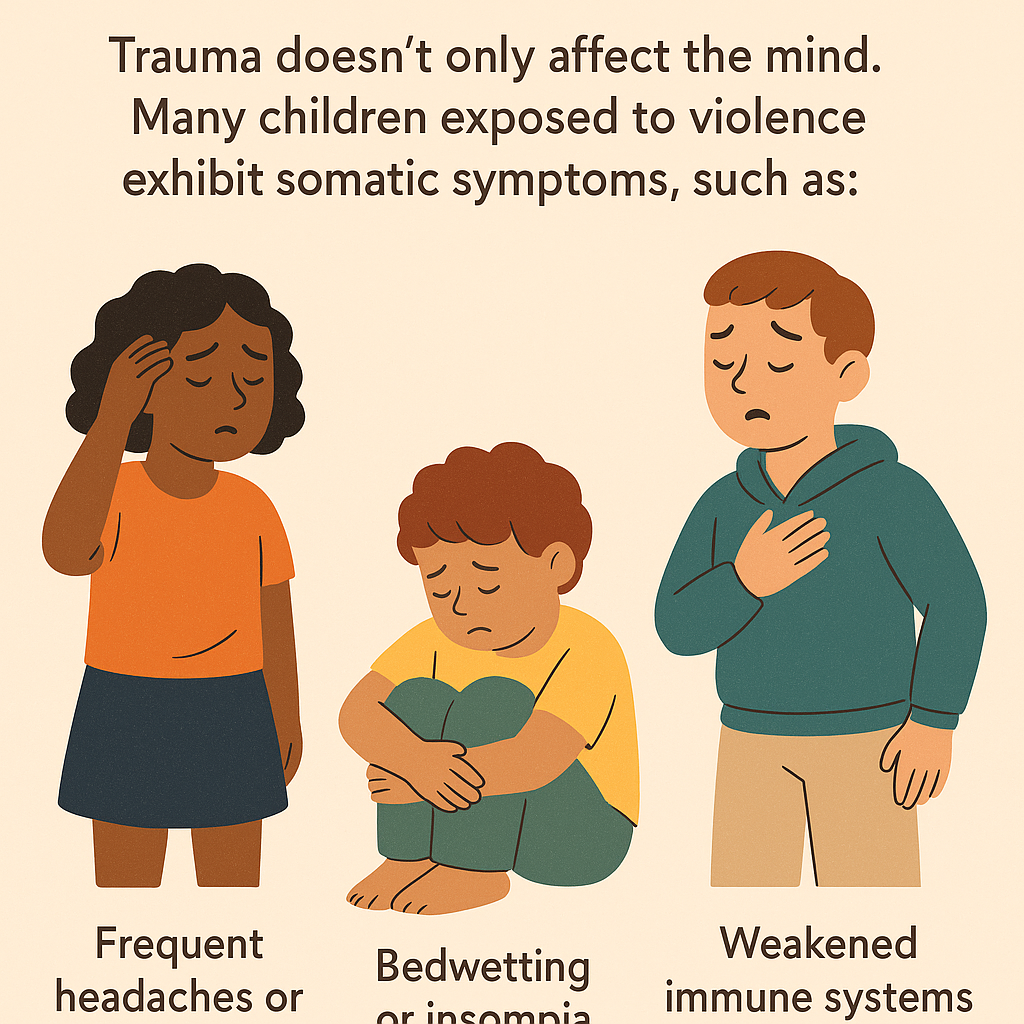
Physical Health Consequences
Trauma doesn’t only affect the mind. Many children exposed to violence exhibit somatic symptoms, such as:
- Frequent headaches or stomach aches
- Bedwetting or insomnia
- Weakened immune systems
- Eating disorders
- Stress-induced physical ailments (e.g., eczema, asthma flare-ups)
Long-Term Psychological Outcomes
Unresolved trauma can echo into adolescence and adulthood. Long-term effects of domestic violence exposure may include:
- Clinical depression or PTSD
- Substance abuse or addiction
- Eating disorders
- Risk-taking behavior (e.g., unsafe sex, reckless driving)
- Perpetuating the cycle of violence (either as a victim or perpetrator)
According to a meta-analysis by Evans, Davies, and DiLillo (2008), children exposed to domestic violence show a moderate-to-high risk of developing internalizing and externalizing disorders.
The “Double Whammy” Effect
Children exposed to both domestic violence and direct abuse face compounded risks. The “double whammy” effect includes significantly higher rates of:
- Depression and anxiety
- Behavioral disorders
- Delinquency and criminal behavior
The Lehigh Longitudinal Study (Moylan et al., 2010) revealed that dual exposure was more predictive of poor adolescent outcomes than either child abuse or domestic violence alone.
Signs to Watch For
Caregivers, teachers, and professionals should be aware of potential red flags:
- Sudden changes in behavior
- Reluctance to go home
- Aggression or bullying
- Emotional withdrawal
- Nightmares or difficulty sleeping
- Risky or self-destructive behavior
No single sign confirms exposure, but patterns of change or distress should raise concern.
Protective and Recovery Factors
Not all children exposed to violence are permanently harmed. With the right interventions, children can recover and thrive.
Key recovery factors include:
- A safe and stable home environment
- Supportive adults (parents, teachers, mentors)
- Trauma-informed therapy or counseling
- School-based support systems
- Opportunities to express themselves (art, sports, music)
- Rebuilding healthy attachments with caregivers
Programs that work with both the child and non-offending parent are often most effective.
Barriers to Healing
Despite the availability of services, children and families face multiple barriers:
- Shame, stigma, or fear of reporting
- Language or cultural obstacles
- Limited access in regional/rural areas
- Lack of affordable or trauma-informed services
These challenges make interagency collaboration essential—between schools, health services, shelters, and child welfare bodies.
Policy and Prevention
Recognizing exposure to domestic violence as a form of child abuse is a crucial policy step. In Australia, it is acknowledged in both state child protection frameworks and the National Framework for Protecting Australia’s Children (2009–2020).
Effective prevention must begin early and include:
- School-based programs on respectful relationships
- Critical reflection on gender roles and violence-supportive attitudes
- Family support services that foster safe parenting
Conclusion: A Call to Action
Domestic violence leaves invisible bruises on children’s hearts and minds. But these wounds don’t have to last forever. With awareness, compassion, and coordinated support, children can overcome trauma and rebuild their lives.
If you suspect a child is affected by domestic violence, don’t wait. Help is available.
Need Help? (Australia)
- 1800RESPECT – 1800 737 732 (24/7)
- Text Support – 0458 737 732
- Video Call Support – 9am to midnight AEST
Internationally:
- Childline (UK) – 0800 1111
- National Domestic Violence Hotline (USA) – 1-800-799-7233
Let’s create safe homes and safer futures—for every child.
Author: Mo Ahmad
Title: Founder, SafeManhood.org – Empowering Men, Supporting Families